Healthcare providers face constant challenges in revenue cycles. Insurers deny Denial Management Appeals frequently. Providers lose billions annually. Effective strategies recover funds. Teams analyze denials quickly. They submit appeals promptly. Automation tools streamline processes. Training enhances staff skills. Prevention reduces future issues. Data drives decisions. Partnerships with payers improve outcomes. Outsourcing offers expertise. Metrics track success rates.
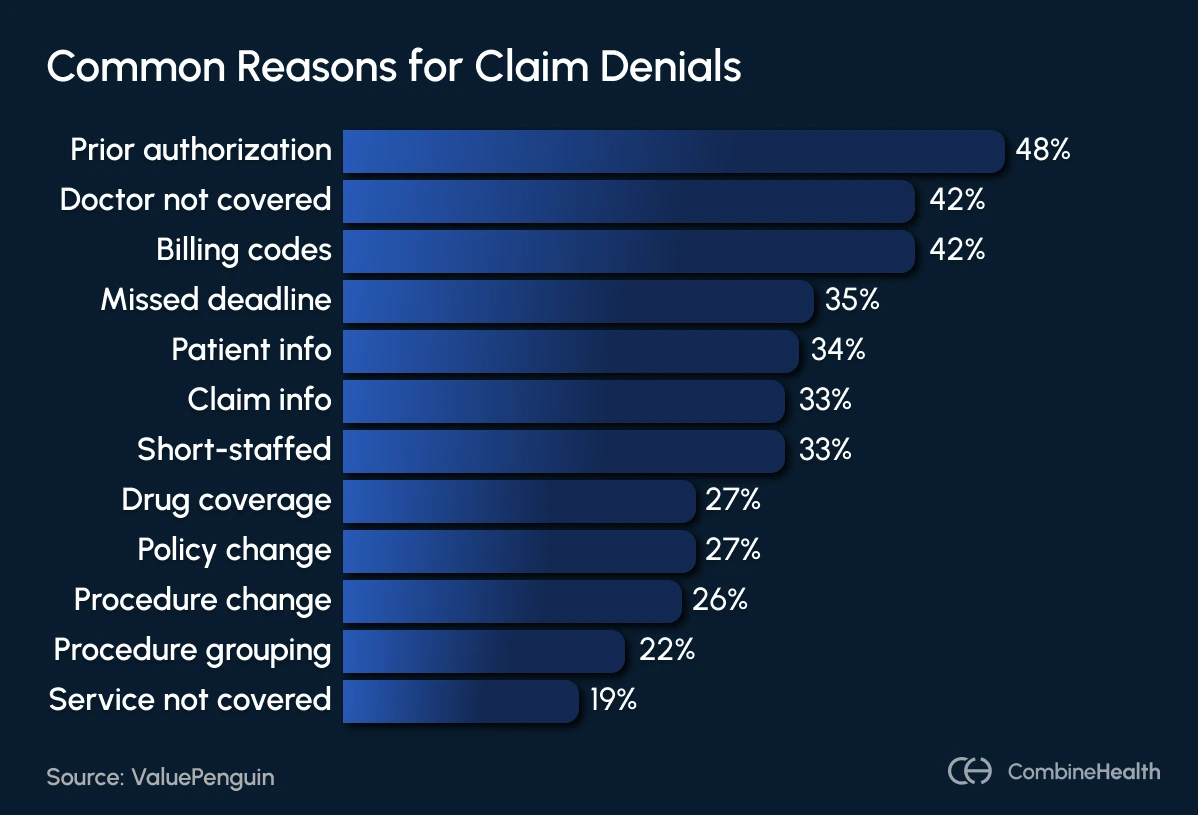
Payers reject claims for various reasons. Coding errors top the list. Providers enter wrong codes. Insurers flag mismatches. Missing information causes rejections. Claims lack patient details. Duplicate submissions occur often. Systems send claims twice. Eligibility issues arise frequently. Patients lose coverage mid-treatment. Timely filing deadlines pass unnoticed. Providers miss submission windows. Medical necessity disputes happen regularly. Services seem unnecessary to payers. Prior authorizations get overlooked. Procedures require pre-approvals. Coordination of benefits confuses teams. Multiple insurers complicate claims. Non-covered services lead to denials. Policies exclude certain treatments. Charge exceeds fee schedules sometimes. Billings surpass contracted rates.
Teams identify denial types first. Hard denials mean no payments. Soft denials allow corrections. Root causes reveal patterns. Analysis uncovers systemic errors. Categorization groups similar issues. Trends emerge from data. Prevention starts here. Staff training addresses gaps. Processes get refined. Technology flags potential problems. Clean claims reduce denials. Verification checks eligibility upfront. Accurate documentation supports claims. Regular audits catch mistakes early.
The Role of Denial Management Appeals
Providers implement denial management appeals to recover revenue. Teams review denied claims thoroughly. They gather supporting documents. Appeals letters argue cases strongly. Deadlines dictate submission timelines. Payers require specific formats. Success depends on evidence. Clinical notes justify services. Policies guide appeal levels. Initial appeals go to insurers. Higher levels involve reviews. External arbitrations occur sometimes. Tracking monitors progress. Follow-ups ensure timely responses. Analysis improves future appeals. Overturn rates measure effectiveness. Teams celebrate wins. Lessons come from losses.
Denial management appeals form core strategies. Providers prioritize high-value denials. They allocate resources wisely. Small denials get batched. Large ones receive attention. Collaboration unites departments. Billing teams work with clinicians. Legal experts assist complex cases. Templates standardize letters. Customization adds details. Persuasive language convinces reviewers. Facts outweigh emotions. Attachments include records. Appeals succeed more often.
Steps in the Denial Management Appeals Process
Teams receive denial notifications first. They log details immediately. Investigation follows quickly. Root causes get identified. Corrections address errors. Resubmissions happen for soft denials. Appeals prepare for hard ones. Documentation compiles evidence. Letters draft arguments. Submissions meet deadlines. Tracking begins post-submission. Follow-ups occur regularly. Decisions arrive eventually. Wins recover payments. Losses prompt reviews. Prevention plans develop next. Processes refine continuously. Metrics evaluate efficiency. Teams adjust tactics.
Identify denial types accurately. Conduct root cause analysis deeply. Prioritize denials strategically. Execute appeals timely. Track outcomes meticulously. Prevent recurrences proactively. Use technology for automation. Train staff on procedures. Partner with experts when needed. Monitor payer trends. Adapt to changes. Improve overturn rates. Boost revenue recovery. Reduce administrative burdens. Enhance financial health.
Common Reasons for Denials and How to Address Them
Coding issues deny claims often. Providers use outdated codebooks. Billers enter wrong digits. Solutions involve regular updates. Training reinforces accuracy. Software suggests codes. Missing data rejects submissions. Forms lack signatures. Patient info stays incomplete. Verification processes fill gaps. Front-end checks catch omissions. Automation populates fields. Duplicate claims waste efforts. Systems resend accidentally. Unique identifiers prevent repeats. Audits detect patterns. Eligibility denials stem from coverage lapses. Patients change insurers. Verification confirms status. Real-time checks avoid surprises. Timely filing misses deadlines. Calendars remind teams. Automation tracks dates. Extensions request when possible.
Medical necessity denials challenge providers. Payers question services. Documentation proves needs. Clinical guidelines support cases. Peer reviews strengthen appeals. Prior authorization absences cause issues. Procedures need approvals. Protocols ensure requests. Tracking monitors responses. Coordination of benefits confuses. Primary payers shift. Updates clarify roles. Communication resolves disputes. Non-covered services exclude payments. Policies dictate coverage. Education informs patients. Alternatives get offered. Fee schedule excesses deny claims. Contracts set rates. Adjustments align billings. Negotiations improve terms.
Best Practices for Denial Management Appeals
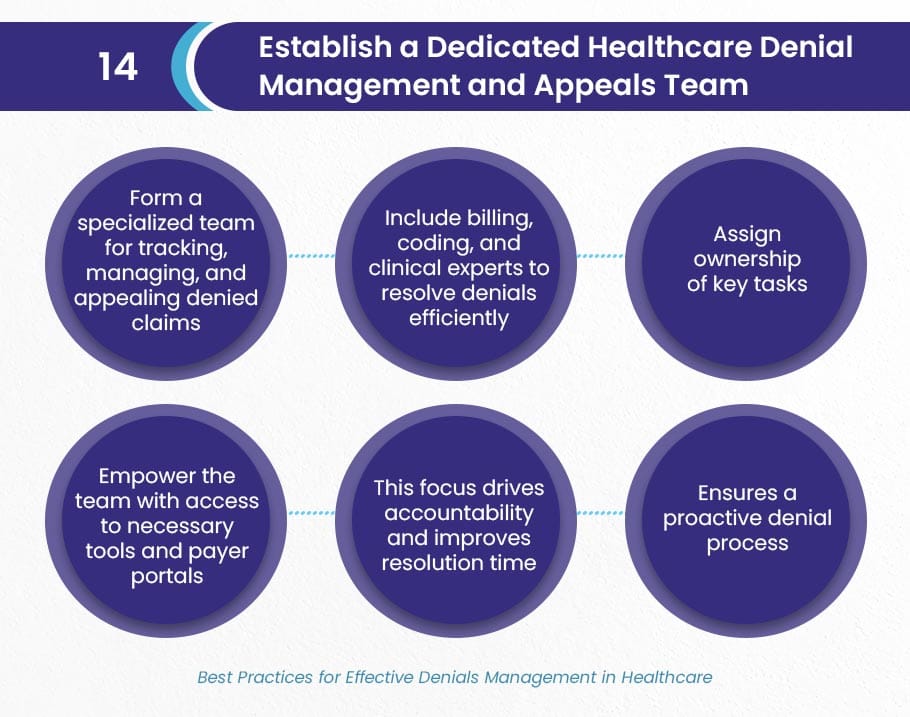
Providers adopt best practices in denial management appeals. Teams categorize denials systematically. They perform root cause analyses. Prioritization focuses efforts. Appeals execute thoroughly. Technology automates tasks. Training builds skills. Outsourcing provides expertise. Metrics guide improvements. Collaboration enhances outcomes. Prevention integrates strategies. Data analytics reveal insights. Process optimizations reduce errors. Staff empowerment boosts efficiency. Payer relationships foster resolutions. Continuous monitoring ensures compliance.
Develop robust documentation practices. Utilize automation for verifications. Streamline appeals with templates. Monitor deadlines strictly. Analyze trends regularly. Educate teams ongoingly. Implement preventive measures. Leverage AI for predictions. Partner with denial specialists. Track key performance indicators. Adjust strategies dynamically. Celebrate successful overturns. Learn from failed appeals. Refine processes iteratively. Achieve higher recovery rates.

Strategies for Successful Appeals
Craft compelling appeal letters. State facts clearly. Back claims with evidence. Argue assertively for reimbursements. Gather comprehensive documentation. Include clinical notes. Attach test results. Provide policy references. Meet timely deadlines. Know payer requirements. Submit via portals. Track appeal statuses. Follow up persistently. Escalate when necessary. Analyze appeal outcomes. Identify successful patterns. Refine arguments accordingly. Train teams on techniques. Use attorney-like approaches. Focus on methodical presentations.
Implement comprehensive education programs. Train on coding accuracy. Educate on documentation needs. Conduct mock appeals. Simulate denial scenarios. Build confidence in teams. Invest in claims software. Automate error detections. Flag potential denials. Integrate with EHR systems. Ensure seamless data flows. Reduce manual interventions. Foster payer collaborations. Build relationships early. Communicate openly. Resolve issues proactively. Share denial insights. Negotiate better terms.
Preventing Future Denials Through Proactive Measures
Providers prevent denials proactively. They verify eligibility real-time. Staff checks coverage upfront. Accurate coding starts early. Guidelines update regularly. Documentation captures details. Clinicians note justifications. Prior authorizations secure approvals. Protocols list requirements. Clean claims submit correctly. Scrubbers review billings. Audits identify weaknesses. Teams correct issues. Training addresses knowledge gaps. Sessions occur frequently. Technology predicts risks. AI analyzes patterns. Alerts flag problems.
Standardize processes across departments. Unite billing with clinical. Align on best practices. Monitor payer policies. Adapt to changes. Educate patients on coverage. Explain potential denials. Offer payment options. Track denial metrics. Set benchmarks for rates. Aim for reductions. Celebrate improvements. Invest in resources. Hire denial specialists. Outsource complex tasks. Focus internal efforts. Achieve sustainable revenue.
Technology’s Impact on Denial Management Appeals
Technology transforms denial management appeals. Automation handles repetitive tasks. Software categorizes denials. AI performs root analyses. Predictive tools forecast issues. Integration connects systems. Data flows seamlessly. Portals submit appeals. Tracking features monitor progress. Analytics provide insights. Dashboards display metrics. Cloud solutions enable access. Security protects information. Mobile apps facilitate updates. Teams respond quickly. Efficiency increases dramatically.
Adopt AI for pattern recognition. Machine learning identifies trends. Algorithms suggest corrections. Bots process resubmissions. Natural language processing reads denials. Extraction pulls key data. Robotics automates letter drafting. Customization adds specifics. Electronic submissions speed delivery. Integrations with payers streamline. Reduce manual errors. Enhance accuracy rates. Boost recovery percentages. Lower administrative costs. Improve overall performance.
Challenges in Denial Management Appeals and Solutions
Teams face increasing denial volumes. Payers tighten rules. Solutions involve scaling resources. Outsourcing handles overflows. Staff burnout occurs often. Workloads overwhelm teams. Rotations provide relief. Training builds resilience. Complex regulations confuse. Policies change frequently. Consultants offer guidance. Subscriptions update knowledge. Appeal timelines pressure. Deadlines loom short. Prioritization eases burdens. Automation reminds teams. Low overturn rates discourage. Failures demotivate staff. Analysis refines strategies. Successes motivate groups.
Resource limitations hinder efforts. Budgets constrain investments. ROI justifies technology. Partnerships share costs. Payer disputes escalate. Resolutions take time. Mediation speeds processes. Documentation gaps weaken cases. Incomplete records fail appeals. Protocols ensure completeness. Interdepartmental silos isolate. Communication breaks down. Collaboration bridges gaps. Unified approaches succeed.
Case Studies: Real-World Success in Denial Management Appeals
Hospitals reduce denial rates significantly. They implement AI tools. Overturns increase by 30%. Revenue recovers millions. Clinics train staff intensively. Coding errors drop sharply. Appeals succeed more often. Practices outsource appeals. Experts handle complex cases. Recovery rates soar high. Systems integrate EHR fully. Data accuracy improves greatly. Denials prevent proactively. Providers partner with payers. Joint reviews resolve issues. Relationships strengthen outcomes. Metrics track progress monthly. Adjustments optimize processes. Success stories inspire teams.
One facility faces high denials. They analyze root causes. Training addresses gaps. Technology automates verifications. Denials fall 25%. Appeals win frequently. Another organization struggles with timelines. Software sets reminders. Submissions meet deadlines. Overturns rise steadily. A third adopts predictive analytics. Risks get flagged early. Prevention saves resources. Revenue stabilizes quickly.
The Future of Denial Management Appeals in Healthcare
Industry evolves rapidly. Regulations tighten further. Technology advances quickly. AI dominates processes. Blockchain secures data. Telehealth introduces challenges. Denials adapt accordingly. Value-based care shifts focus. Outcomes drive payments. Prevention gains importance. Collaboration becomes key. Payers and providers unite. Shared data reduces disputes. Training emphasizes compliance. Certifications validate skills. Metrics define success. Benchmarks set standards. Innovation drives efficiency. Future promises better recoveries.
Providers prepare for changes. They invest in education. Teams learn new tools. Strategies evolve dynamically. Focus shifts to prevention. Appeals become rarer. Revenue cycles smooth out. Financial health improves. Patient care enhances. Administrative burdens lighten. Industry thrives overall.
Frequently Asked Questions(FAQs)
What defines denial management appeals?
Providers use denial management appeals to challenge denied claims. They submit evidence to insurers. Processes recover lost revenue. Teams follow structured steps.
Why do claims get denied commonly?
Insurers deny claims for coding errors. Missing data causes rejections. Eligibility issues arise often. Timely filing misses deadlines. Medical necessity disputes occur.
How can providers prevent denials?
Teams verify eligibility upfront. They ensure accurate coding. Documentation supports services. Prior authorizations secure approvals. Audits catch errors early.
What steps involve successful appeals?
Identify denial reasons first. Gather supporting documents. Draft compelling letters. Submit on time. Track and follow up.
How does technology aid denial management appeals?
Software automates categorizations. AI analyzes roots. Portals submit appeals. Analytics track metrics. Predictions prevent issues.
What metrics measure appeal success?
Overturn rates indicate effectiveness. Recovery amounts show impact. Denial reductions track prevention. Timelines evaluate efficiency. Trends guide improvements.

