Experts define the pes anserine bursa as a small sac. It sits inside the knee. This structure cushions tendons and bones. Inflammation often strikes athletes. Runners face higher risks. Obesity worsens the issue. Osteoarthritis links to it too. Diabetes patients report more cases. Proper care prevents problems. Treatment eases pain fast. Knowledge aids recovery.
This article explores anatomy deeply. It covers functions clearly. Common conditions appear next. Symptoms guide early detection. Causes reveal risk factors. Diagnosis uses simple tests. Treatments range from rest to therapy. Prevention strategies build strength. FAQs answer key questions. Readers gain full insights.
What is the Pes Anserine Bursa?
The pes anserine bursa acts as a lubricant. It reduces friction in knees. Fluid fills this tiny sac. Tendons glide smoothly over bones. Irritation causes swelling quickly. Pain follows inflammation always. Bursitis names the condition precisely. Medial knee hosts this bursa. Three muscles connect here tightly. Daily movements stress it often. Overuse triggers issues commonly. Early intervention stops progression.
Patients notice tenderness first. Swelling appears on inner knees. Activities worsen discomfort rapidly. Rest relieves symptoms temporarily. Ice helps reduce inflammation. Compression supports the area. Elevation drains excess fluid. Doctors recommend these steps. Physical therapy strengthens muscles. Stretching improves flexibility. Injections provide relief sometimes. Surgery remains rare.
Anatomy of the Pes Anserine Bursa
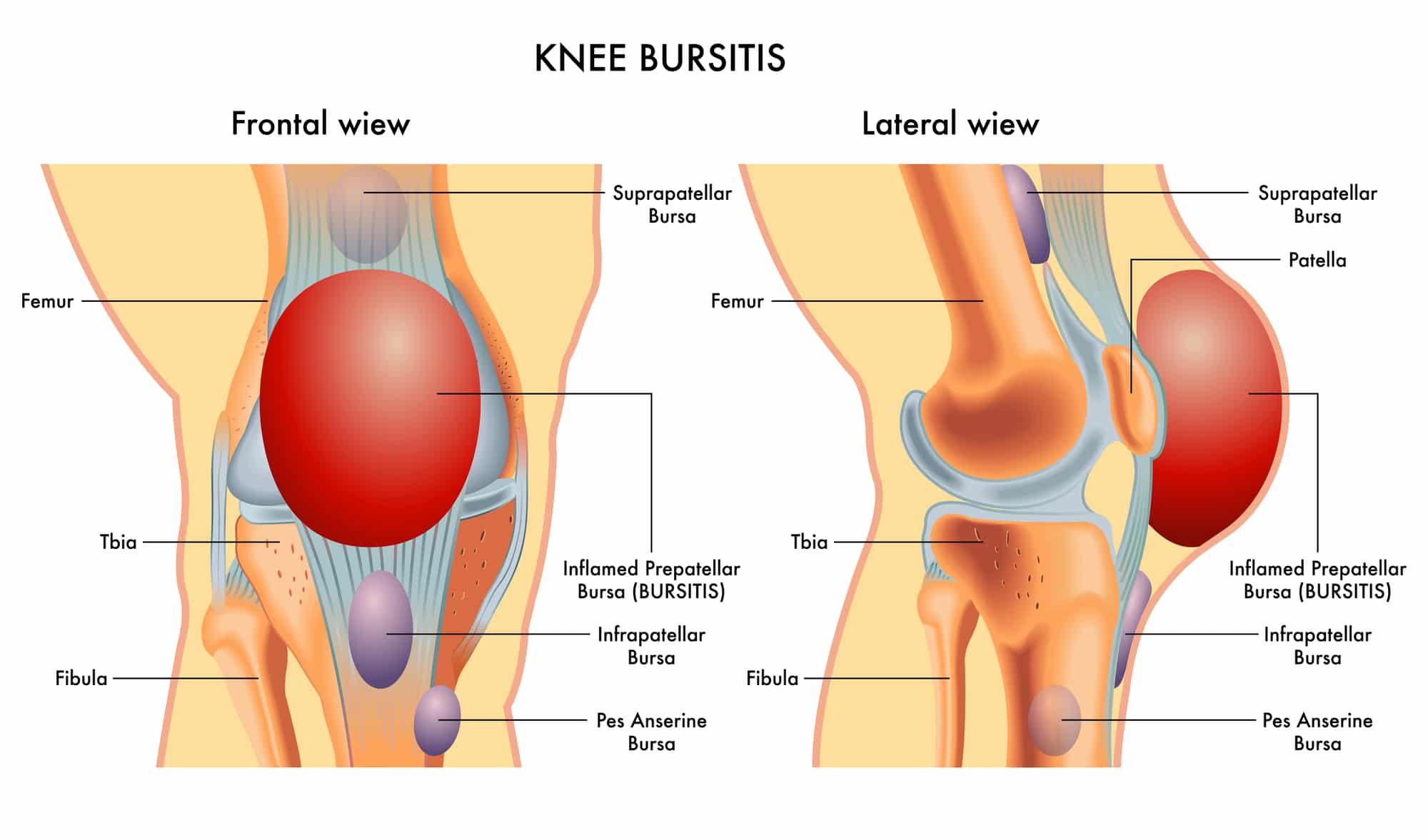
Three tendons form the pes anserine. Sartorius starts from hips. Gracilis runs along thighs. Semitendinosus belongs to hamstrings. They conjoin at medial tibia. This spot resembles goose feet. Latin term “pes anserinus” describes it. Bursa lies beneath these tendons. It separates them from bone. Medial collateral ligament neighbors it. Proximal tibia anchors the structure. Depth measures about 5 cm below joint line.
Bones involved include tibia mainly. Femur connects above indirectly. Patella stays uninvolved typically. Muscles pull during flexion. Tendons insert anteromedially. Bursa cushions repetitive motions. Fluid inside prevents rubbing. Inflammation alters this balance. Swelling presses nearby tissues. Pain radiates from there. Diagrams show clear positions.

The pes anserine bursa measures small. It spans 2-3 inches typically. Location sits 2 inches below joint. Inner knee feels it easily. Palpation detects tenderness. Ultrasound visualizes fluid levels. MRI shows detailed structures. Variations exist among people. Some have larger bursae. Others face congenital issues. Genetics influence susceptibility. Age affects resilience. Middle-aged women report more. Youthful athletes strain it often.
Function of the Pes Anserine Bursa
The pes anserine bursa cushions movements. It allows smooth tendon gliding. Synovial fluid lubricates surfaces. Friction drops during activities. Knee flexion relies on it. Internal rotation benefits too. Stability comes from this setup. Muscles work without hindrance. Daily tasks proceed easily. Sports demand more from it. Running stresses the bursa repeatedly. Jumping adds impact forces.
Bursa absorbs shocks effectively. It protects underlying bones. Tendons avoid wear and tear. Inflammation disrupts this role. Swelling limits motion ranges. Pain signals overuse clearly. Rest restores normal function. Therapy rebuilds strength around it. Prevention maintains its health. Proper warm-ups prepare it. Stretching keeps tendons flexible. Strength training supports the area. Overall fitness enhances performance.
Common Conditions: Pes Anserine Bursitis
Inflammation defines pes anserine bursitis. Bursa swells with excess fluid. Pain hits inner knees hard. Tenderness increases on palpation. Swelling appears visibly sometimes. Activities aggravate the issue. Stairs cause sharp discomfort. Running worsens symptoms fast. Rest eases the pain. Ice reduces inflammation quickly. Compression helps control swelling. Elevation aids fluid drainage.
Bursitis links to tendinopathy often. Tendons inflame alongside bursa. Overuse sparks both conditions. Trauma contributes in some cases. Infections rarely occur here. Chronic issues tie to arthritis. Osteoarthritis erodes joint cartilage. Obesity loads extra pressure. Diabetes impairs healing processes. Women face higher risks. Middle age heightens vulnerability. Athletes monitor for early signs.
Symptoms of Pes Anserine Bursitis
Pain strikes medial knees primarily. It worsens with knee bending. Straightening triggers discomfort too. Tenderness localizes below joint line. Swelling bulges the area. Warmth indicates inflammation. Redness shows severe cases. Stiffness limits morning movements. Walking feels awkward initially. Running provokes sharp pains. Climbing stairs intensifies symptoms. Descending adds more stress.
Night pain disturbs sleep often. Kneeling presses the bursa. Squatting strains it further. Sports halt due to agony. Daily chores become challenging. Weakness affects leg strength. Instability risks falls. Limping alters gait patterns. Compensation strains other areas. Back pain follows sometimes. Hip issues arise too. Full assessment catches all symptoms. Early recognition speeds recovery.
Causes and Risk Factors
Overuse causes most cases. Runners repeat motions excessively. Athletes train without rest. Tight hamstrings pull tendons. Weak hips misalign knees. Obesity adds joint load. Osteoarthritis wears cartilage down. Diabetes slows tissue repair. Trauma impacts the area. Infections invade rarely. Poor biomechanics contribute. Flat feet alter strides. Valgus knees stress medially.
Women report more incidents. Middle age brings risks. Type 2 diabetes links strongly. Sports like soccer strain it. Basketball involves quick turns. Wrestling adds direct blows. Volleyball demands jumps. Improper shoes worsen issues. Uneven surfaces challenge stability. Sudden activity increases spike risks. Genetic factors play roles. Family history matters. Awareness reduces occurrences.
Diagnosis Methods
Doctors take detailed histories. They ask about pain onset. Activities trigger questions. Physical exams palpate tenderness. Swelling checks come next. Range tests motion limits. Strength assesses muscle power. Gait observes walking patterns. Provocation maneuvers replicate pain. Ultrasound images fluid buildup. MRI rules out tears. X-rays spot bone issues.
Blood tests exclude infections. Aspiration drains fluid sometimes. Lab analysis confirms diagnosis. Differential includes meniscus tears. MCL sprains mimic symptoms. Arthritis overlaps often. Tendinitis confuses cases. Expert evaluation clarifies. Orthopedists specialize here. Sports medicine aids athletes. Timely diagnosis prevents worsening. Tools enhance accuracy.
Treatment Options
Rest halts aggravating activities. Ice applies 20 minutes hourly. Compression wraps support knees. Elevation raises legs above heart. NSAIDs reduce pain inflammation. Acetaminophen eases discomfort too. Physical therapy stretches hamstrings. Strengthening targets quads hips. Ultrasound therapy soothes tissues. Massage loosens tight muscles. Braces stabilize joints. Orthotics correct foot issues.
Corticosteroid injections relieve severe cases. PRP promotes healing naturally. Surgery removes bursa rarely. Bursectomy resolves chronic issues. Rehab follows operations. Gradual return builds strength. Lifestyle changes manage weight. Diet aids diabetes control. Activity modification prevents recurrence. Home exercises maintain gains. Follow-ups monitor progress. Multidisciplinary approaches work best.

Prevention Strategies
Warm-ups prepare muscles tendons. Stretching lengthens hamstrings daily. Strengthening builds hip stability. Core exercises enhance balance. Proper footwear supports arches. Gradual training avoids overloads. Rest days allow recovery. Cross-training varies activities. Weight management reduces loads. Diabetes control minimizes risks. Biomechanical assessments fix issues. Orthotics help flat feet.
Regular check-ups catch problems early. Hydration keeps tissues healthy. Nutrition fuels muscle repair. Sleep aids overall recovery. Technique coaching refines movements. Coaches guide athletes safely. Trainers design balanced programs. Awareness educates on limits. Listening to body prevents injuries. Consistent habits sustain health. Prevention outperforms treatment always.
Frequently Asked Questions (FAQs)
What causes pain in the pes anserine bursa?
Overuse inflames the sac. Tight muscles strain it. Obesity adds pressure. Arthritis links to issues. Sports trigger repetitive stress.
How do doctors diagnose pes anserine bursitis?
They review activity history. Exams check tenderness swelling. Ultrasound shows fluid. MRI rules out other problems. Blood tests exclude infections.
What treatments help pes anserine bursitis?
Rest eases initial pain. Ice reduces swelling fast. Therapy strengthens muscles. Injections provide quick relief. Surgery handles rare cases.
Can exercise prevent pes anserine issues?
Stretching keeps tendons flexible. Strengthening builds support. Warm-ups prepare knees. Cross-training varies loads. Proper form avoids strain.
Who faces higher risks for bursitis?
Runners encounter overuse often. Obese individuals load joints. Diabetic patients heal slowly. Middle-aged women report more. Athletes in high-impact sports.
When should someone see a doctor?
Persistent pain signals issues. Swelling limits motion. Night discomfort disturbs sleep. Activities worsen symptoms. Early visits speed recovery.