Doctors use vad ventricular devices to support failing hearts. These mechanical pumps assist blood circulation in patients with severe heart failure. Hospitals implant them surgically for long-term or temporary aid. Patients experience improved quality of life after implantation. Researchers develop these devices to bridge gaps in organ transplants.
Ventricular assist devices save lives daily. They pump blood when hearts weaken. Surgeons connect them to heart chambers. Batteries power the external components. Medical teams monitor patients closely post-surgery.
What Is a Vad Ventricular?
A vad ventricular acts as a mechanical pump. It helps the heart’s lower chambers. The device takes over pumping duties. Patients with weakened hearts benefit greatly. Implantation occurs in specialized centers.
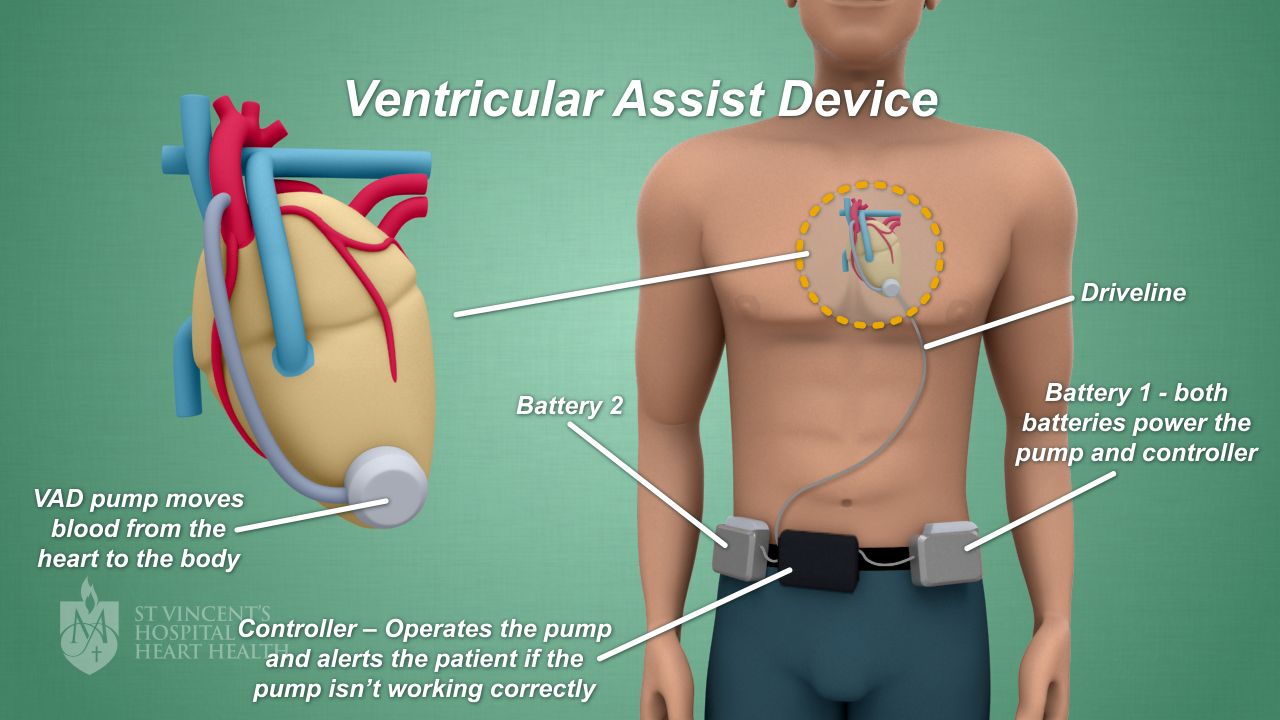
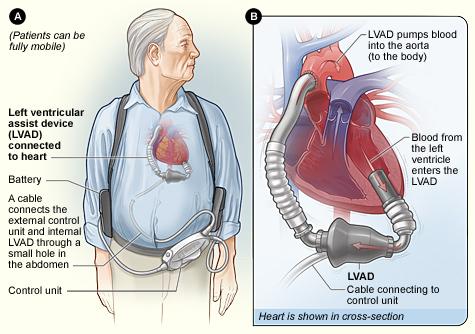
The vad ventricular includes an internal pump. Tubes connect it to the heart. An external controller manages operations. Batteries provide portable power sources. Doctors program the device for optimal flow.
Types of Vad Ventricular Devices
Left ventricular assist devices dominate the field. They support the left heart chamber. Right ventricular devices aid the right side. Biventricular devices help both chambers. Each type addresses specific failures.
Left devices pump oxygenated blood outward. Right devices send blood to lungs. Biventricular setups combine both functions. Surgeons choose based on patient needs. Technology advances improve all types.
Temporary devices offer short-term support. Permanent ones serve as destination therapy. Bridge-to-transplant devices prepare for heart replacement. Recovery devices allow heart healing. Innovation drives type diversification.
How Vad Ventricular Works
The vad ventricular pulls blood from ventricles. It propels blood into major arteries. Continuous flow models maintain steady circulation. Pulsatile models mimic natural heartbeats. Sensors adjust flow rates automatically.
Internal components reside in the chest. Drivelines exit through the skin. External packs hold batteries and controllers. Alarms alert to malfunctions. Patients learn to manage daily operations.
Blood enters the pump inlet. Impellers or pistons move the fluid. Outflow grafts connect to aorta. Anticoagulants prevent clotting inside. Regular checkups ensure proper function.
Indications for Vad Ventricular Implantation
Doctors recommend vad ventricular for end-stage heart failure. Patients unresponsive to medications qualify. Those awaiting transplants use it as bridge. Inoperable candidates receive destination therapy. Severe cardiomyopathy often necessitates implantation.
Acute myocardial infarctions lead to consideration. Congenital defects prompt early use. Post-cardiotomy shock requires temporary support. Chemotherapy-induced damage benefits from aid. Evaluation teams assess eligibility thoroughly.
Symptoms like fatigue trigger assessments. Shortness of breath indicates need. Swelling in extremities signals failure. Low ejection fractions confirm severity. Multidisciplinary reviews decide implantation.
The Implantation Procedure
Surgeons perform open-heart surgery for implantation. They access the chest cavity. Pumps attach to ventricular apex. Grafts sew into aorta. Drivelines tunnel through abdominal wall.
Anesthesia ensures patient comfort. Cardiopulmonary bypass supports during attachment. Testing verifies device function. Closure follows successful integration. Recovery starts in intensive care.
Post-op monitoring detects issues early. Medications control pain and infection. Physical therapy begins gradually. Discharge planning includes education. Follow-up visits schedule routinely.
Risks and Complications of Vad Ventricular
Infections pose major risks at driveline sites. Bleeding occurs from anticoagulants. Strokes result from blood clots. Device malfunctions require urgent fixes. Right heart failure complicates some cases.
Gastrointestinal bleeding affects patients. Arrhythmias disrupt normal rhythms. Hemolysis damages red blood cells. Pump thrombosis blocks flow. Vigilant care minimizes these issues.
Patients report driveline discomfort. Battery failures strand users. Allergic reactions to materials happen rarely. Long-term use leads to aortic insufficiency. Teams manage complications proactively.
Benefits and Outcomes
Vad ventricular extends life expectancy significantly. It improves exercise tolerance. Patients resume daily activities. Quality of life scores rise post-implantation. Hospital readmissions decrease over time.
Survival rates reach 80% at one year. Bridge patients transplant successfully. Destination therapy sustains indefinitely. Energy levels boost dramatically. Emotional well-being enhances with independence.
Studies show reduced heart failure symptoms. Organ perfusion optimizes bodily functions. Weight management becomes easier. Sleep patterns normalize. Social interactions increase for users.
Living with a Vad Ventricular
Patients carry external components daily. They change batteries regularly. Showering requires protective covers. Travel plans accommodate equipment. Support groups offer shared experiences.
Diet focuses on heart-healthy foods. Exercise programs build strength. Medication adherence prevents clots. Emergency protocols prepare for alarms. Family training ensures assistance.
Routine clinic visits monitor parameters. Blood tests check coagulation levels. Imaging assesses device position. Lifestyle adjustments promote longevity. Community resources aid adaptation.
Care and Maintenance
Users clean driveline sites meticulously. They inspect for infection signs. Controllers log performance data. Technicians service equipment periodically. Replacement parts stock at home.
Anticoagulation therapy balances risks. Blood pressure management optimizes flow. Hydration supports circulation. Avoidance of magnetic fields protects. Education empowers self-care.
Psychological Impact
Implantation alleviates physical burdens. Anxiety about device failure persists. Counseling addresses emotional challenges. Positive outlook correlates with better outcomes. Peer networks reduce isolation.
Body image concerns arise from scars. Independence restores confidence. Achievement milestones celebrate progress. Mental health screening integrates care. Resilience builds over time.
Advances in Vad Ventricular Technology
Engineers design smaller pumps. Wireless power transfers eliminate drivelines. Biocompatible materials reduce clotting. Smart sensors predict failures. Clinical trials test innovations.
Full maglev technology suspends impellers. Reduced hemolysis improves safety. Longer battery life enhances mobility. Integration with pacemakers synchronizes. Future models aim for total implantation.
Research focuses on pediatric applications. Stem cell combinations aid recovery. AI optimizes flow adjustments. Global access expands programs. Cost reductions broaden availability.
History of Development
Inventors pioneered pulsatile devices in 1960s. Continuous flow models emerged later. FDA approvals marked milestones. Clinical trials proved efficacy. Adoption grew worldwide.
Key devices include HeartMate series. HeartWare offered compact designs. Evolution decreased sizes. Survival improved iteratively. Ongoing refinements continue.
Global Perspectives on Vad Ventricular
Developed nations lead implantation rates. Training programs standardize procedures. Reimbursement policies influence access. Cultural attitudes affect acceptance. International registries track outcomes.
Emerging markets build expertise. Collaborations share knowledge. Device costs challenge equity. Humanitarian efforts donate equipment. Global studies compare results.
Patient Stories and Testimonials
Survivors share recovery journeys. One patient hiked mountains post-implant. Families express gratitude for extra time. Challenges build character. Success inspires others.
Communities host awareness events. Media features life-changing stories. Testimonials highlight resilience. Hope motivates candidates. Narratives humanize technology.
Role in Transplant Programs
Vad ventricular bridges to transplantation effectively. It stabilizes patients on waitlists. Organ allocation prioritizes supported cases. Post-transplant removal occurs smoothly. Programs integrate seamlessly.
Donor shortages necessitate alternatives. Destination therapy fills gaps. Hybrid approaches combine options. Outcomes rival transplants in select groups. Strategies evolve with data.
Economic Considerations
Implantation costs exceed $100,000 initially. Long-term savings reduce hospitalizations. Insurance covers most expenses. Value-based care evaluates benefits. Economic models project savings.
Government funding supports research. Philanthropy aids underserved patients. Cost-benefit analyses guide policies. Affordability improves with scale. Investments yield societal returns.
Ethical Issues
Allocation decisions raise fairness questions. Informed consent ensures understanding. End-of-life planning addresses deactivation. Resource distribution debates equity. Guidelines govern practices.
Patient autonomy respects choices. Quality versus quantity weighs heavily. Cultural beliefs influence decisions. Ethics committees review cases. Frameworks evolve with technology.
Training for Healthcare Providers
Surgeons master implantation techniques. Nurses specialize in device management. Technicians handle maintenance. Multidisciplinary teams coordinate care. Simulation labs enhance skills.
Continuing education updates knowledge. Conferences share best practices. Certification programs standardize expertise. Mentorship builds proficiency. Quality improvement drives excellence.
Research and Clinical Trials
Studies evaluate new device generations. Trials test biocompatibility enhancements. Data registries compile long-term results. Collaborative efforts accelerate progress. Funding prioritizes innovation.
Endpoints measure survival and quality. Adverse events track safety. Comparative effectiveness researches alternatives. Patient-reported outcomes inform designs. Evidence guides clinical decisions.
Pediatric Applications of Vad Ventricular
Children receive scaled-down devices. Congenital defects prompt use. Growth considerations adapt designs. Family support integrates care. Outcomes improve survival rates.
Challenges include size constraints. Infection risks heighten vigilance. School integration promotes normalcy. Long-term data accumulates slowly. Specialization advances field.
Comparison with Other Therapies
Medications manage early failure stages. Pacemakers address rhythm issues. CRT devices synchronize contractions. Transplants offer definitive cures. Vad ventricular fills advanced niches.
Cost comparisons favor devices long-term. Availability surpasses organs. Risks differ by modality. Patient selection optimizes choices. Combined therapies enhance results.
Future Directions
Miniaturization promises total implantation. Bioengineered components reduce rejection. Personalized devices match anatomies. Telemedicine monitors remotely. Integration expands applications.
Regenerative medicine complements support. Gene therapies target causes. Nanotechnology refines mechanics. Sustainability focuses on durability. Visionaries predict widespread use.
Conclusion
Vad ventricular transforms heart failure treatment. It offers hope where options dwindle. Patients thrive with proper support. Advances promise brighter futures. Adoption continues to grow globally.
Healthcare evolves with these innovations. Teams dedicate to patient success. Communities benefit from extended lives. Research fuels ongoing improvements. Commitment drives progress forward.

